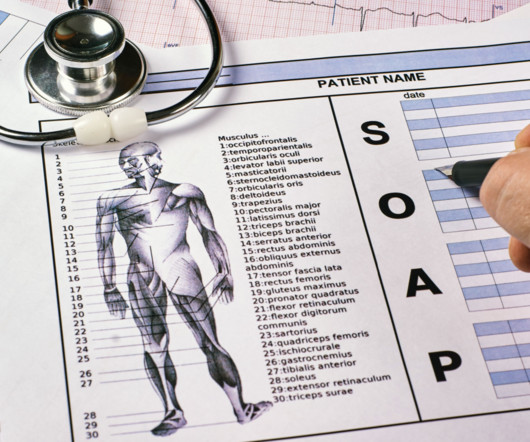
What Are SOAP Notes and How Do You Write Them?
Valant
JULY 24, 2024
The information recorded may include symptoms, medical history, test results, diagnoses, treatment plans, prescription medications, and progress made at appointments. Check out Valant’s clinical documentation features to learn more. This information is shared with insurance companies to justify claims.









Let's personalize your content