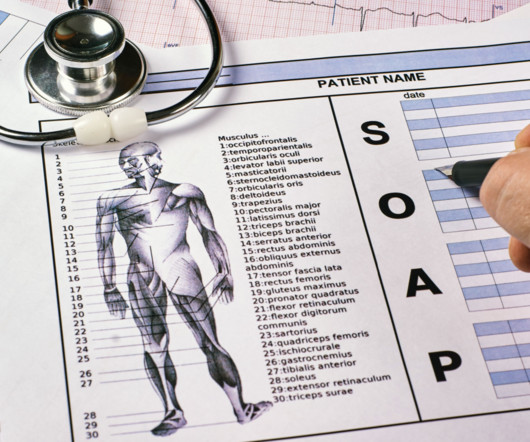
What Are SOAP Notes and How Do You Write Them?
Valant
JULY 24, 2024
The SOAP note is typically specific to one therapy session and includes information such as: Subjective : Basic patient history and items reported by the patient, such as concerns, symptoms, medical history, and medications. Note Items of a particularly private nature may be reserved for private therapy notes (not progress notes).







Let's personalize your content