5 issues in the check-in process that impact your medical practice
Health Prime
NOVEMBER 20, 2024
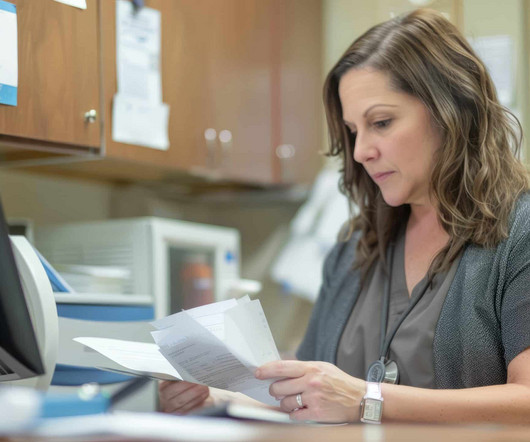
In this stage of the medical billing process, your front-end staff ensures proper collection and recording of valuable data essential to provide proper services to the patient and ensure their coverage. Poor communication Effective communication is crucial during your revenue cycle process; however, check-in is paramount.













































Let's personalize your content