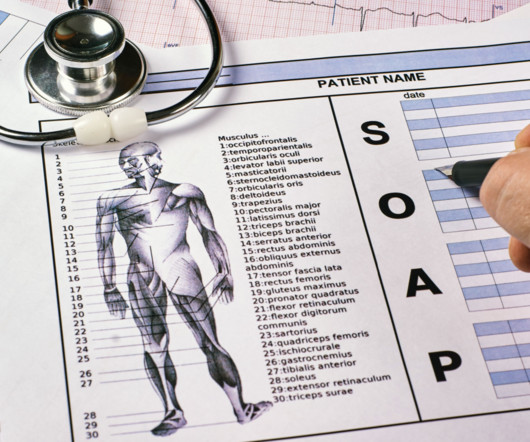
What Are SOAP Notes and How Do You Write Them?
Valant
JULY 24, 2024
The information recorded may include symptoms, medical history, test results, diagnoses, treatment plans, prescription medications, and progress made at appointments. SOAP notes can help you stay on-track during appointments with patients and quickly complete your notetaking after the session has ended.

































Let's personalize your content